“How bad does it hurt?” It’s not for nothing that doctors usually struggle to ascertain our level of pain. It depends not only on how bad we report it to be, but also on the amount of pain we think we feel.
But are there reasons behind it that would begin to decipher our (in)ability to cope with or even verbalize the dreaded sensation? According to a recent collaborative study led by Dr. Elia Valentini from the University of Essex, there’s more to this phenomenon than a mere lack of tools that would accurately quantify exactly how much pain there is in an “ouch.”
What Does Our Brain Do While We Hurt?
So far, science held a more or less persisting view that a surefire way to quantify our levels of pain – much like any other physical sensation or state – was to measure our brain’s electrical activity. When you’re sitting and idly scrolling on your phone, your brain waves will likely hover around 12 Hz. Start dozing off and these alpha waves will slide back in intensity to theta (4-8 Hz) or even delta (1-4 Hz) if you were to fall asleep.
But if a very angry tweet kicks you out of your zen, your brain waves are likely to surge into the beta sphere, anywhere from 22 to 38 Hz. Finally, if you hop into the kitchen and stub your toe on the way, your brain activity will shoot through the roof and exhibit a very high level of oscillations, up to 80 Hz.
Or so the theory went!
The study published in the Journal of Neurophysiology paints a more nuanced picture. Different brains, it suggests, show remarkably varied responses to the same type and amount of pain. This leads the researchers to believe that each of us have our own and unique “pain fingerprint.” To gauge what our brain does against what it says it does, the researchers took two groups of willing subjects and put them through two datasets. The first group of willing participants was zapped with a laser and touched within a 2-week span, whereas the other only only got the laser stimulus. All the while, the participants’ response was measured on two fronts. Their EEG was recorded with a focus on the rapid gamma brain waves. Three seconds after the stimulus was applied, the participants were asked to verbally rate their feeling of pain from no pain (0) to maximum pain they were willing to tolerate (10).
The most intriguing finding? We may experience and describe a stimulus as painful in a certain way and to a certain extent, but the gamma waves will not necessarily play along. In other words, the waves that have been associated with pain for so long will actually vary significantly between individuals. But where they do show in an individual, they will be remarkably stable, consistent and reproducible.
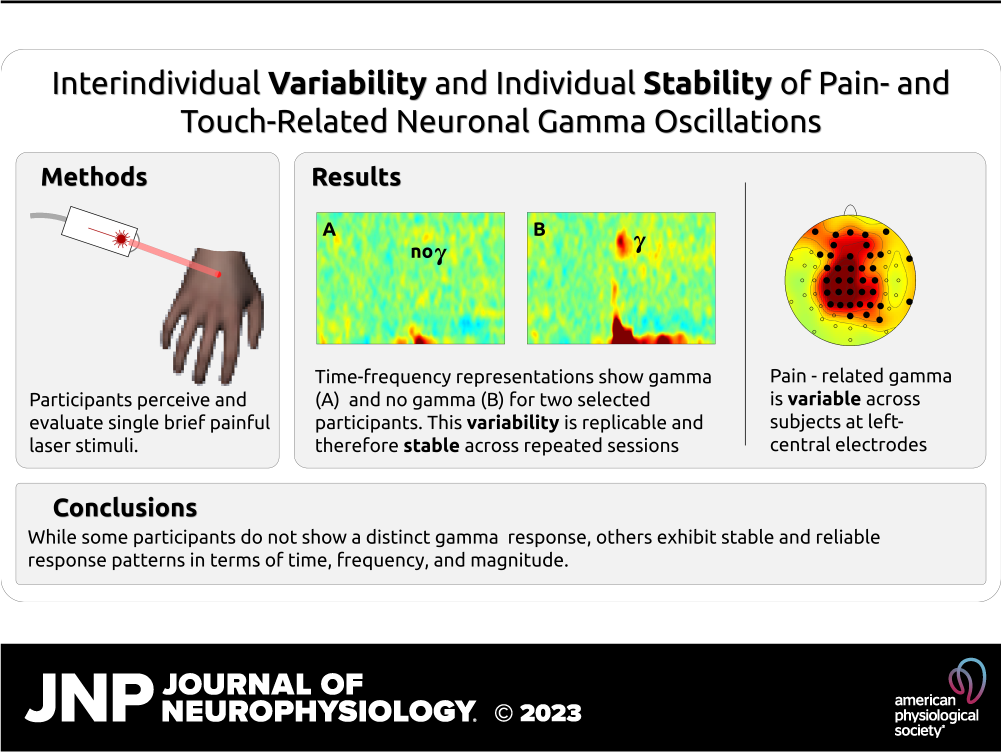
For example, if Peter and John were to stub their toes 10 times with exactly the same amount of force, both will likely perceive and report the pain as maximum. But their brain activity may show a different picture. Whereas Peter’s brain is buzzing with gamma waves, John’s remains calm. No matter how many times they take part in this toe-stubbing contest, the study indicates, both Peter’s and John’s brain waves will remain mutually inconsistent, but true to their own form.
Now, this could make the research seem like a case against the role of gamma waves in our dealing with pain. But it’s more than that. As the first author points out, it’s yet another scientific reminder that two things don’t have to cause one another just because they coincide. “The study acts as a timely reminder that even when a strong group-level correlation is replicated by several studies, we may still be fooled in drawing causal interpretations,” Dr. Valentini told Medical News Today. He also hopes that this research will set the stage for other studies that could result in designing personalized painkillers and other meds that wouldn’t only rely on our ability to articulate our pain.